Many nursing home patients die of sepsis. Often, this does not result in a nursing home lawsuit because the infection occurred without negligence from a nursing home. But, too often, sepsis is the result of a bedsore or other preventable condition because of nursing home negligence or neglect. With nursing home sepsis, there are often signs that show an infection if the nursing home staff is paying attention.
Our lawyers handle nursing home sepsis lawsuits where a death occurs because the patient was not properly diagnosed and treated. This page talks about sepsis and the settlement value of sepsis wrongful death nursing home lawsuits.
What Is Sepsis?
Sepsis is an extremely dangerous and often fatal medical condition in which an infection becomes so advanced that it invades the bloodstream, and the body’s immune system begins to damage its own organs. Sepsis is essentially the result of a person’s immune defense system being overrun. Well over a million cases of sepsis are reported in the U.S. each year, and 250,000 people die from it on an annual basis.
Sepsis Nursing Home Statistics
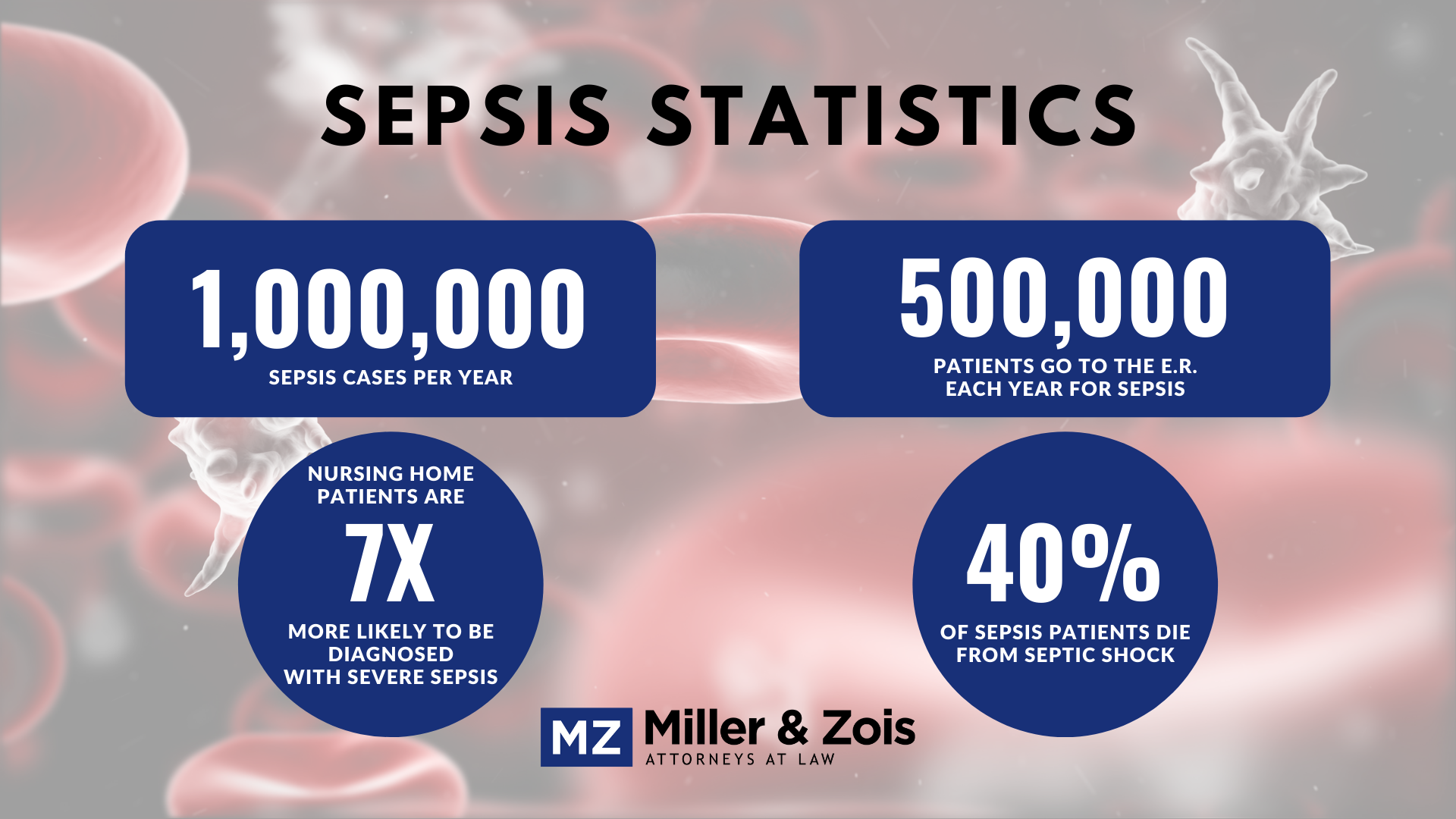
Nursing home sepsis statistics are very daunting for a topic few people focus on until they have a parent or spouse dealing with sepsis:
- Nursing home residents are seven times greater risk for severe sepsis diagnosis than non-nursing home residents (14% vs. 1.9%)
- Half a million patients go to the ER with severe sepsis every year in the U.S.
- There are one million sepsis cases a year
- 40% of patients that have sepsis that goes into septic shock die
What Are the Stages of Sepsis?
Sepsis develops in 3 distinct phases: (1) sepsis, (2) severe sepsis, and (3) septic shock. Sepsis is something that often occurs in severe cases of medical malpractice or nursing home neglect. This post will explain and describe the 3 phases of sepsis infections.
 STAGE I: Sepsis
STAGE I: Sepsis
The first stage of sepsis appears when patients with an infection develop a specific set of signs and symptoms that indicate that the infection has progressed into sepsis. The preliminary symptoms for any sepsis diagnosis include:
- Fever: a very high body temperature (above 100 degrees) is always a sign of a significant infection because the body’s internal temperature rises when it tries to fight off bacteria.
- Infection: while fever is a sign of systemic infection, other infections (e.g., an infected cut, or urinary tract infection) have more localized symptoms such as redness and swelling or pain and discomfort.
- Mental Decline: an acute downward change in mental capacity such as being confused or “dazed” and unable to process information or move normally.
- Extreme Illness: severe body pain and discomfort, shortness of breath, and other severe types of illness symptoms.
If two or more of these initial signs and symptoms are present, a diagnosis of stage one sepsis can be made if any combination of the following additional diagnostic criteria is present:
- Inflammatory Symptoms: inflammatory response symptoms consistent with sepsis include very high white blood cell count, abnormal levels of “immature” white blood cells, and elevated levels of procalcitonin (PCT) and plasma C-reactive protein.
- Hemodynamic Symptoms: hypotension (low blood pressure), low mixed venous or central venous oxygen saturation levels, high cardiac index.
- Organ Malfunction Symptoms: low urine output, high creatinine in the blood, abnormal blood clotting, high bilirubin levels, and low platelets.
STAGE II: Severe Sepsis
The second stage of sepsis is known as severe sepsis. Severe sepsis occurs when there are clear signs of organ dysfunction and tissue hypoperfusion. The following diagnostic indicators are used to identify when sepsis has progressed into severe sepsis (stage 2):
- Hypotension: hypotension (low blood pressure) would be systolic pressure below 90 mm Hg and arterial pressure under 70 mm Hg, or an overall decrease in systolic pressure of 40 mm Hg or more.
- Lactate Elevated: abnormally high levels of lactate in the blood is a sign that an infection interferes with normal organ function, causing excess lactate to accumulate.
- No Urine Output: if the patient is consuming fluids but not urinating it can be another sign that their organs are not fully functioning.
- ARDS: Acute Respiratory Distress Syndrome (“ARDS”) is a condition in which respiratory failure and malfunction are caused by acute lung inflammation.
- Platelet Count: a very low blood platelet count is a sign of severe sepsis, suggesting poor organ functioning.
- Changes in Skin Color
This combination of symptoms will only be used to reach a diagnosis of severe sepsis when they are clearly the result of stage I sepsis (not related to a preexisting condition). The symptoms should also be seen to continue even after fluid replacement.
STAGE III: Septic Shock
The third and final stage of sepsis is called septic shock. Septic shock occurs when multiple vital organs in the body begin shutting down entirely. The diagnostic symptoms of septic shock are the same as those listed above for severe sepsis, except that septic shock is usually characterized by a sudden and dramatic drop in blood pressure and a spike in lactic acid levels in the blood. Septic shock symptoms:
- Acute Hypotension: systolic blood pressure drops below 65 mm Hg and cannot be maintained above that level without medication.
- Lactic Acid Spike: extremely high levels of lactic acid in the blood will indicate that oxygen is not being distributed to organs by the blood cells.
Sepsis in Elderly Patients
Elderly people are particularly vulnerable to sepsis because the human immune defense system weakens as we get older. Older people are also much more likely to have chronic medical issues like diabetes, cancer, kidney disease, and other issues that can further weaken and undermine the immune system.
Sepsis in elderly patients most commonly originates from either a respiratory infection such as pneumonia or a urinary tract infection, both of which are very common in older people. Bedsores (also known as pressure sores) are also a common source of infections that can lead to sepsis in elderly patients. Nursing home neglect is a common cause of bedsores and when not properly treated they can lead to infections and sepsis.
Can Bedsores Lead to a Sepsis Infection?
An adequately treated bedsore should not cause a sepsis infection. The problem is that nursing homes often do not identify and do the little things necessary to treat a bedsore. This turns a minor problem into one that can be fatal.
Can Sepsis Be Effectively Treated by a Nursing Home?
If sepsis is diagnosed early only in its progression, it can be effectively treated with antibiotics and fluid replacement. If the condition is not promptly diagnosed, however, it can become too advanced for treatment to work.
How Long Does It Take to Die from Sepsis?
Severe sepsis can potentially cause organ failure and death within just a few days without any treatment. Even if sepsis does not cause death within the first few weeks, it can have lingering effects and indirectly contribute to death months and even years after the initial infection. Approximately 40% of patients who survive the first month of sepsis will die within the next 2 years.
Can Nursing Home Neglect Cause Sepsis?
Yes, a nursing home can be a setting where sepsis may occur, especially if proper care and hygiene standards are not maintained. In nursing homes, residents are often at a higher risk for infections due to factors such as age, weakened immune systems, and the presence of chronic medical conditions. Familiar sources of infection in such environments include:
- Urinary Tract Infections (UTIs): Often associated with the use of catheters.
- Respiratory Infections: Including pneumonia, which can be more common in elderly populations or those with preexisting lung conditions.
- Skin Infections: These include pressure ulcers or bedsores, which can become infected if not properly cared for.
- Gastrointestinal Infections can be caused by bacteria like Clostridioides difficile, often due to the overuse or misuse of antibiotics.
- Wound Infections: Especially in residents with surgical wounds or diabetic ulcers.
Sometimes, it is just as simple as ensuring residents are washing their hands or washing them for patients.
A recent study has uncovered that nursing home residents taking antibiotics and not practicing regular hand washing are at an increased risk of contracting infections from antibiotic-resistant bacteria.
Researchers found that 75% of surfaces in nursing home residents’ rooms harbored vancomycin-resistant enterococci (VRE), a particularly stubborn and dangerous antibiotic-resistant bacteria. The study highlights the heightened vulnerability of residents who had used antibiotics within the past month and neglected hand hygiene, making them more susceptible to challenging bacterial infections.
So if these infections are not promptly or adequately treated, they can lead to sepsis. This is why it’s crucial for nursing homes to have strict infection control policies and for staff to adhere to high standards of hygiene and care. Recognizing early signs of infection and responding appropriately is critical to preventing the development of sepsis in nursing home residents.
Nursing Home Sepsis Verdicts and Settlements
Below are summaries of recent verdicts and settlements involving sepsis cases at nursing homes.
- $150,000 Settlement (Pennsylvania 2023): A 60-year-old woman was admitted to a nursing home and rehab facility after undergoing abdominal hernia surgery. While at the nursing she developed a sepsis infection and died. A wrongful death lawsuit alleged that the facility was negligent in allowing the infection to develop, and the case settled.
- $29,515,246 Verdict (South Carolina 2023): A 73-year-old female resident of a nursing home died due to sepsis while under the care and custody of the facility. At the time of her death, the decedent’s body was covered with decubitus ulcers and she was undernourished at five feet tall and 89 pounds. The nursing home sepsis lawsuit alleged that the defendants failed to take action to prevent decubitus ulcerations and other skin problems.
- $30,950,000 Verdict (California 2023): An 86-year-old man fell at home was admitted to a nursing home. At home he was neglected during his two-week stay at the facility and developed two unstageable heel pressure sores, one of which was discovered to be a to-the-bone stage IV pressure sore. He eventually died from sepsis.
- $375,000 Settlement (Pennsylvania 2022): An elderly resident at a nursing home outside Philadelphia was reportedly diagnosed with sepsis after he developed a Stage IV right sacral decubitus ulcer that required surgical debridement. His sacral wounds persisted when he was transferred back to the defendants’ nursing home, and approximately two months later, he was diagnosed with septic shock from his sacral decubitus ulcer and had developed additional pressure wounds.
- $250,000 Settlement (Illinois 2021): A 77-year-old woman died due to sepsis and a sacral decubitus ulcer while she was a resident of a nursing home operated by defendant Manor Care Health Services Inc. he estate alleged that the defendants were negligent in failing to prevent and properly treat the decedent’s decubitus ulcers, which became infected and caused or contributed to her death, failing to provide proper follow-up care, and failing to properly supervise her, among other failures.
Legal Assistance for Nursing Home Negligence in Maryland
Pursuing a legal claim against a nursing home goes beyond seeking compensation; it’s about holding these facilities accountable for their actions.
Our civil justice system mandates financial restitution in cases where negligence in nursing homes results in harm. However, these claims serve a broader purpose. The threat of legal action is a key factor in ensuring nursing homes adhere to standards of care and safety. Without the deterrent of potential lawsuits, the safeguards for protecting nursing home residents could be severely compromised.
If you or a loved one has suffered due to nursing home negligence, Miller & Zois are here to help. Contact us at 800-553-8082 or get a free consultation online, and we’ll discuss your options and how we can assist in seeking justice and compensation.
 Maryland Injury Law Center
Maryland Injury Law Center