Fetal macrosomia is a medical term that means fetal weight at birth is greater than 4000 grams (8 lbs. 13 oz). Compared to the size of other newborns of the same gestational age, this is considered excessive fetal growth. Your doctor will be concerned with the baby’s probable weight at delivery for a few reasons and should want more testing to be done.
Fetal macrosomia is a serious condition in pregnancy. It is well recognized in the medical literature that a major concern in the delivery of a macrosomic baby is shoulder dystocia and the attendant risks of permanent brachial plexus palsy. It requires close monitoring and frequent visits to the doctor’s office. But the reward is a healthier baby at delivery and sometimes a healthier mother, too.
Why is Fetal Macrosomia Important?
To put it simply, bigger babies have more birth complications.Most people know that smoking in pregnancy can lead to low birth weight for the newborn. But the opposite—a very big baby—can also be dangerous.
When the expectant mother has certain health problems like diabetes, the fetus stores more fat than is necessary. This extra fat will give the child larger shoulders, which can complicate a normal delivery with shoulder dystocia. These babies are called large for gestational age or LGA. It can also change the way the newborn handles his own blood sugar right after delivery.
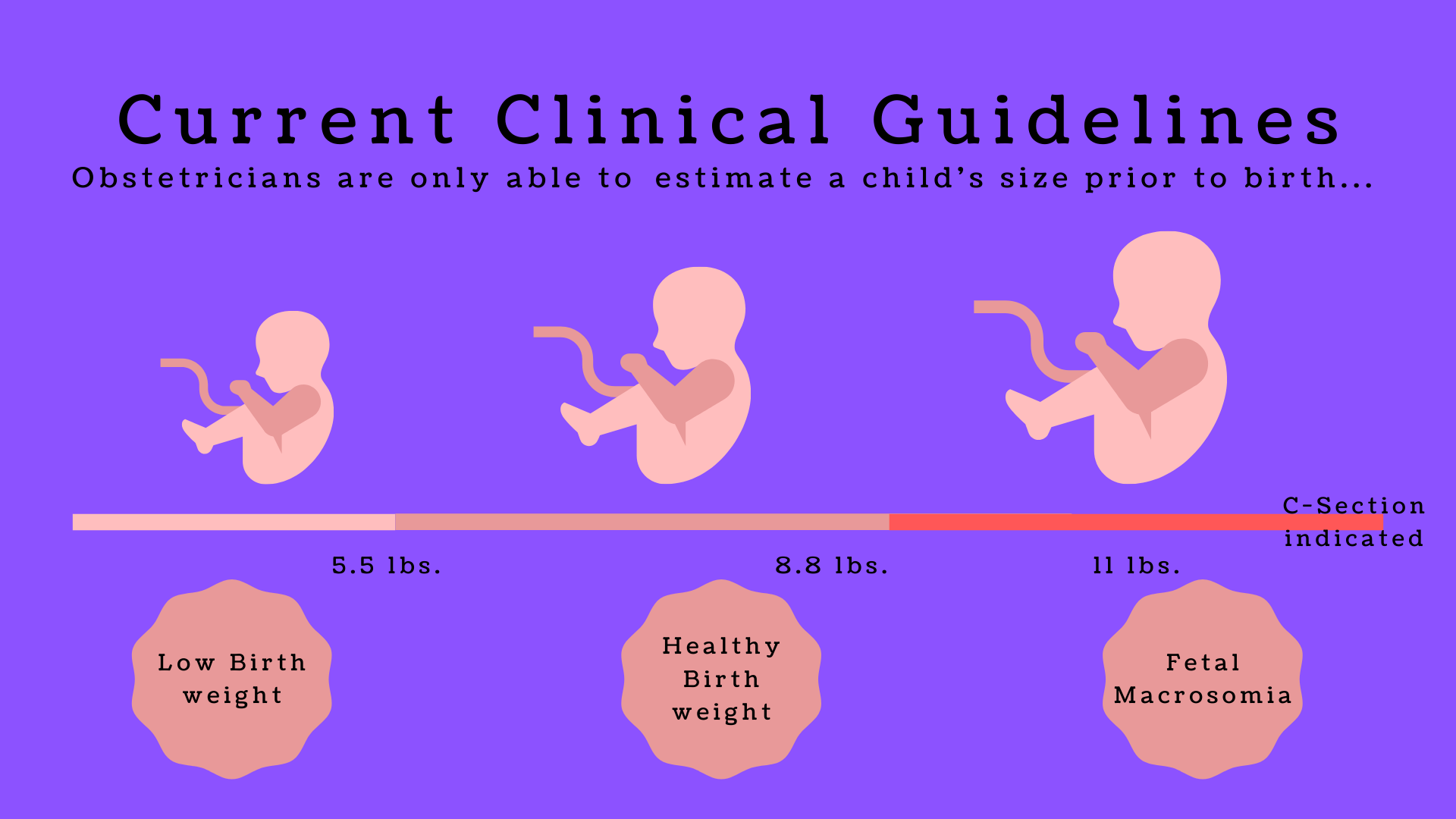
However, studies have shown that the risk of complications depends on many factors. Doctors are no longer routinely ordering Cesarean sections just because a baby is big. New standards address all the issues before considering surgery.
Predicting which baby will have birth complications from their weight and size is not an exact science. This is because shoulder dystocia can happen even with a small baby. What obstetricians know is that the higher the weight, the more problems can happen.
How Many Babies are LGA?
About 9% of living newborns weigh over 4,000 grams at birth. Babies can also weigh over 4,500 grams (9 lbs., 10 oz), but this is unusual. A baby who weighs over 5000 grams (11 pounds) is rare.
Around 20 weeks of pregnancy, the expectant mother’s fundal height—the distance between her pubic bone and the top of her uterus—will reflect how many weeks she has been pregnant. This will give her care provider a baseline to compare how fast the fetus is growing. The health care provider will firmly press around the uterus (Leopold’s maneuvers) to determine the position and size of the fetus. If the fundal height and fetal size measure larger than usual according to the weeks of pregnancy, the mother will be sent for an ultrasound.
New studies show that an ultrasound may not predict LGA and a prenatal exam.
But an ultrasound of the fetal size is most valuable during the first 4-5 months of pregnancy. It can tell the doctor how fast the fetus is growing. Detecting rapid fetal growth can also help the doctor see another danger in pregnancy.
Gestational Diabetes
The most common cause of fetal macrosomia is diabetes, especially gestational diabetes.
In gestational diabetes, the mother’s hormones make her body less able to metabolize blood sugar. Sugar is present in every carbohydrate that the body breaks down, and the mother’s cells become resistant to the insulin that her body produces.
These hormones are present in every pregnancy, and the exact reason they block the action of insulin is unknown. Some research shows the process may help to direct more nutrients to the growing fetus. Whatever purpose it has in human biology, the reality now is that every woman should be tested for gestational diabetes. This screening should take place between 24-28 weeks of pregnancy.
Some women are more vulnerable to gestational diabetes. Occasionally, an expectant mother has undiagnosed type 2 diabetes before she became pregnant. When she is diagnosed at a prenatal visit, what appears to be gestational can be type 2 diabetes that can continue after delivery of the baby. The hormones in pregnancy are the same, however, and her blood sugar can be more difficult to control.
Mother’s Weight and Baby’s Weight
If a woman has obesity before she becomes pregnant, this also puts her fetus at risk for fetal macrosomia.
Obesity is defined as an adult body mass index of 30 or higher and can cause multiple health issues even without pregnancy. Many women with obesity have tried to lose weight, but dieting during pregnancy is not recommended.
To decrease the risk of an LGA baby, the mother with obesity has a few options. First, her doctor or midwife needs to talk with her about nutrition during pregnancy. A pregnant woman only needs to eat 300 additional calories more per day than a non-pregnant woman.
Those 300 calories should not come from sodas or junk food! Fresh fruits, vegetables, lean meats, whole grains, and portion control are important. The right eating plan for an obese pregnant woman is not so different from a regular nutritious diet.
The second option for the obese expectant mother is mild exercise. Exercise in obese pregnant women has been shown to decrease the risk of pregnancy hypertension, delivery complications, and gestational diabetes. Some exercises appropriate for pregnancy are walking, swimming, and low-intensity aerobics (no bouncing). Strenuous exercising is not recommended. Also, because certain conditions in pregnancy do not allow exercise, she needs to get her doctor’s approval before starting.
A large fetal size is not always preventable. A few other causes include genetics (big babies are common in the family), ethnicity, and pregnancy with a male fetus.
One indicator of a macrosomic baby is if her fundal height was greater than the gestational age. Usually, gestation age by dates is equivalent to the fundal height. If the baby is larger than its age, there is an real chance for a macrosomic baby.
A Difficult Birth
When the mother has high blood sugar, it crosses the placenta to reach the fetus. To handle this extra glucose from the mother, the fetus makes more insulin. When this happens, the extra insulin can lead to the fetus storing more fat. More fat results in a bigger baby and a greater chance of birth complications.
When a mother is laboring with an LGA baby, the labor can take longer than normal. When the baby is too high in the pelvis for too long, the doctor will want a C-section. This is not for the doctor’s convenience—it also concerns the safety of mother and baby.
A long labor can make the mother too exhausted to push. And if labor moves along as it should, and the fetus descends into the birth canal, a more severe complication can happen.
Doctors have a few medical terms to describe it, but this is what it means: the baby gets stuck during delivery. It is called shoulder dystocia because the shoulders cannot pass through the birth canal. It is also called cephalopelvic disproportion (CPD) because the baby is bigger than the mother’s pelvis can accommodate.
When it happens, the doctor only has a few choices.
The doctor will perform an episiotomy to make more room for the baby. Although episiotomies are not as common in modern medicine, they are recommended in a birthing emergency. A vacuum or forceps will also be used to assist the baby to come out. During this time, the mother must pull her knees to her chest (the nurse can help her). This is the McRoberts position, and it can relieve pressure on the baby’s shoulder.
If the baby still cannot come out of the birth canal, the doctor will order an immediate C-section. A few C-sections are performed in under 10-15 minutes if the situation is critical. When the surgery is performed this fast, it has a higher danger of complications for mother and baby. However, they are done to prevent oxygen deprivation of the fetus and brain damage.
Better Outcomes with LGA
Early education and treatment are crucial in reducing complications from fetal macrosomia. Prompt prenatal care and diagnosis can make a difference in the delivery. Communication between doctor and patient is vital during pregnancy.
A birthing plan before going into the hospital is a good idea. The doctor or midwife needs to talk with the mother about birthing risks and complications. As mentioned earlier, many shoulder dystocia incidents occur with babies that are not LGA, but the mother needs to be prepared if this happens.
The Home Birth
According to the American College of Nurse-Midwives, prenatal care from a midwife can reduce the need for a C-section. Midwifery has also been linked with greater patient satisfaction about pregnancy care. Laws vary from state to state regarding home births in the United States. However, fetal macrosomia meets the definition of a high-risk pregnancy. It can cause an emergency C-section. A home birth is never recommended by the American College of Obstetricians and Gynecologists for any pregnancy.
If prenatal care by a midwife is desired by the expectant mother, the midwife needs to work with the doctor. For the safety of mother and baby, the LGA baby should be delivered in the hospital.
 Maryland Injury Law Center
Maryland Injury Law Center