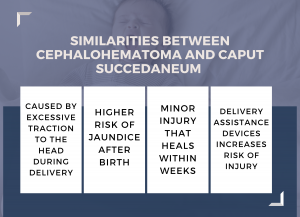
Caput succedaneum and cephalohematoma are similar – but distinct – birth injuries that cause a baby’s head to swell.
While there are important differences between caput succedaneum and cephalohematoma, the common thread between the two is they both scare parents but they are typically not serious and will heal themselves over a relatively short period.
My Child Has Caput Succedaneum and I’m Worried… What Should I Do?
For most concerned parents, you should know that caput succedaneum and cephalohematoma are not a big deal when not coupled with a brain bleed or other cerebral insult. So many people reading this are parents who have been told their child has caput succedaneum. When it is your newborn child — and I have four myself — it is easy to panic. But the good news is that in the vast majority of cases, caput succedaneum ends up being insignificant and it resolves on it own without intervention.
The bad news is that these conditions can lead to more severe complications in the absence of a health care provider’s prompt diagnosis, vigilance, and effective treatment. The possibility that one of these conditions is connected with or arising from a more serious birth injury also means that immediate medical attention should be given to diagnosing and providing any necessary treatment for these conditions.
You can not underscore enough the importance of prompt and effective diagnosis and treatment of caput succedaneum or cephalohematoma. What would otherwise have been harmless can grow to become a more serious —sometimes lifelong — condition on account of medical negligence. This can arise from failing to recognize the issue during or after delivery, a failure to provide proper treatment (such as a C-section, when warranted), or even failing to diagnose precipitating causes of the injuries before birth.
If your child has suffered from one of these conditions because of medical neglect, you should be eligible to receive compensation. Contact me if you are looking for answers about your child’s case.
Let’s look at the most common questions about caput succedaneum and cephalohematoma.
What is caput succedaneum?
 Caput succedaneum is a birth injury characterized by swelling or edema to a baby’s scalp observable shortly after delivery, as caused by pressure on a baby’s head. This swelling of the newborn scalp extends across the edematous region above the periosteum that crosses suture lines where the bony plates of the skull join together. (In contrast, neonatal cephalohematoma does not cross the suture lines.)
Caput succedaneum is a birth injury characterized by swelling or edema to a baby’s scalp observable shortly after delivery, as caused by pressure on a baby’s head. This swelling of the newborn scalp extends across the edematous region above the periosteum that crosses suture lines where the bony plates of the skull join together. (In contrast, neonatal cephalohematoma does not cross the suture lines.)What causes caput succedaneum?
- Protracted active labor course
- Operative vaginal delivery, especially vacuum-assisted delivery, which is the most significant risk factor for developing caput succedaneum and scalp injury.
- Oligohydramnios
- Primigravida pregnancy
- Braxton-Hicks contractions
- Premature rupture of membranes.
What are the symptoms of caput succedaneum?
The most prominent symptom of caput succedaneum is puffiness under the skin of the scalp. As a result, your baby’s head might appear to be abnormally large, bulging around the affected area. Once the swelling goes down, the baby’s head resumes its normal shape. Some additional, less common changes which can affect the appearance of your baby’s head include:
- Bruising (and/or color changes) of the baby’s scalp
- Increased molding (elongation) of the baby’s head
Doctors typically express caput succedaneum in terms of these changes in appearance, and symptoms of minor discomfort. But there is a risk that more serious complications can arise along with or because of the condition.
The most important of these for you to know is newborn jaundice, which is characterized by a yellowish-green skin pigmentation because of bilirubin accumulation. If treated immediately, there are typically no long-term problems that will arise from jaundice. But untreated, jaundice can lead to long-term complications such as kernicterus, a kind of brain damage which can cause:
- Hearing loss
- Athetoid cerebral palsy
- Impaired tooth enamel development
- Permanent upward gaze
Also, if there is a skull fracture underneath your baby’s swelling or if bleeding is extensive, the risks posed by caput succedaneum can be much more serious which is why a full, prompt diagnosis is medically warranted.
How is caput succedaneum diagnosed?
What is the treatment for caput succedaneum?
What is cephalohematoma?
Cephalohematoma is like caput succedaneum, as both conditions are birth injuries characterized by swelling in a baby’s head. It is a clinical diagnosis. So there is no definitive test for cephalohematoma.
What causes cephalohematoma?
- An infant’s head is larger than their mother’s pelvic area
- Use of an epidural
- Difficult and prolonged labor
What are the symptoms of cephalohematoma?
The most obvious symptom of cephalohematoma is a soft, unusual bulge on the back of your baby’s skull. Because of its location under the periosteum, you will probably not see any cut or bruise on the surface of the skin over the bulge.
Expect the bulge to feel harder as the blood calcifies and then shrinks and disappears after a few weeks under normal circumstances. Aside from this bulge, there are often no additional (or obvious) symptoms as a result of cephalohematoma. However, cephalohematoma can cause your child to develop other conditions, such as:
- Jaundice (yellowing)
- Anemia (low red blood cell counts)
- Hypotension (low blood pressure)
- Meningitis
- Infection (such as osteomyelitis)
- Skull Deformation
Furthermore, if accompanied by a more serious condition such as a skull fracture, cephalohematoma can also lead to the growth of this fracture into a leptomeningeal cyst.
Although cephalohematoma is typically not a serious condition, if these other conditions arise from or accompany it there is a possibility that your child may experience developmental delays, motor skill deficiencies, and a non-resolution of the condition. In more acute instances, long-term risks include the development of cerebral palsy. For this reason, your child must be promptly diagnosed and provided with any necessary treatment for this condition, even though it is typically only a minor affliction.
How is cephalohematoma diagnosed?
What is the treatment for cephalohematoma?
When a newborn has a cephalohematoma, the best treatment is to wait and let the body naturally reabsorb the collected fluid. Typically, your child will see the bump resolve and the cephalohematoma will go away on its own within three months. Physicians will not need to provide any treatment unless additional complications arise. In rare cases, the cephalohematoma may not resolve and calcification or ossification may occur. If the cephalohematoma has not disappeared after 6 weeks, a skull x-ray or CT scan may be necessary.
Draining a cephalohematoma
Sometimes, the physician may recommend draining the accumulated blood. This is usually not recommended but it makes sense in some cases.
Complications such as infections and/or abscess formations can arise from draining. If the condition results in a lowering of your baby’s red blood cell count (anemia), additional treatment such as a blood transfusion may become necessary.
Jaundice and Cephalohematomas
Just like with caput succedaneum, newborns are more prone to jaundice because a a cephalohematoma can cause jaundice (skin yellowing) in newborns because the clotted blood in the cephalohematoma can interfere with the normal process of breaking down and eliminating bilirubin, a yellow pigment produced when red blood cells break down.
Bilirubin typically travels through the bloodstream and is processed by the liver, but if there is a buildup of bilirubin, it can cause the skin, eyes, and other tissues to appear yellow, a condition known as jaundice. This can occur when the blood from a cephalohematoma interferes with the liver’s ability to break down and eliminate bilirubin, leading to an increased level of bilirubin in the blood and resulting in jaundice. It is important for newborns with cephalohematoma to be carefully assessed for jaundice and treated promptly if necessary.
Should the condition result in jaundice, light therapy, intravenous immunoglobulin, or exchange transfusion may be prescribed.
Newborns with cephalohematomas have a higher risk of developing jaundice in the first days after birth, so they need to be monitored for yellow discoloration of the skin, eyes, or mucous membranes. If they show signs of jaundice, a test to measure their bilirubin level will be done.
Can jaundice be a big deal? Yes. But in most cases, it goes away as easily a cephalohematomas do.
Treating hardened cephalohematomas
There is debate about the best way to treat cephalohematomas that have hardened and formed a clear outer and inner layer of bone. Some believe that early surgery is better, while others believe it is not necessary unless there are other clinical indications.
In patients with later-stage ossification or calcification, surgery may be necessary to improve the outcome, decrease the risk of elevated intracranial pressure, and improve the appearance. The surgical technique involves removing the overlying newly formed bone, the soft tissue mass, and the underlying original bone. The depressed region can then be remodeled as a bone graft.
Cephalohematomas can be treated safely with surgery, such as craniotomy or craniectomy and cranioplasty, and have good outcomes with minimal evidence in the following years.
How long does cephalohematoma last?
What is a subdural hematoma?
What is caput-medusae?
Why is Caput Succedaneum Usually Harmless?
Caput succedaneum is usally harmless because it does not place pressure on the brain. the collection of blood is sitting above the skull, not under it where it might put pressure on the brain.
 Maryland Injury Law Center
Maryland Injury Law Center